MedicationsWhat they do
Antiplatelet drugs:
|
Reduce blood clotting They do this by making the cells in your blood, known as platelets, less “sticky”. This lowers the chance of another clot forming. |
 |
Anticoagulants:
|
Reduce blood clotting Anticoagulants interrupt part of the process involved in the formation of blood clots stopping your blood from clotting as quickly or easily. This lowers the chance of another clot forming.If you are taking an anticoagulant you should be issued with either an alert card or booklet specific to the drug you have been prescribed. It is important that you carry this on you so that in case of emergencies, a doctor attending to you knows which anticoagulant you are taking and at what dose. |
 |
Statins:
|
Lower cholesterol If you have a high cholesterol level, fatty deposits can start to build up in blood vessels and increase your risk of stroke. Statins work by reducing the amount of cholesterol in your blood by blocking the chemical in the liver that produces it. |
 |
| Blood Pressure medication: | Lower Blood Pressure If you have high blood pressure you may have been given a tablet to help lower it. These tablets may cause side effects, but they are doing an important job in helping to lower your risk of another stroke or heart attack. To find out more about high blood pressure treatments and medications see more information |
 |
Key point
As every patient and stroke is different, medication is tailored to meet each individual’s needs.










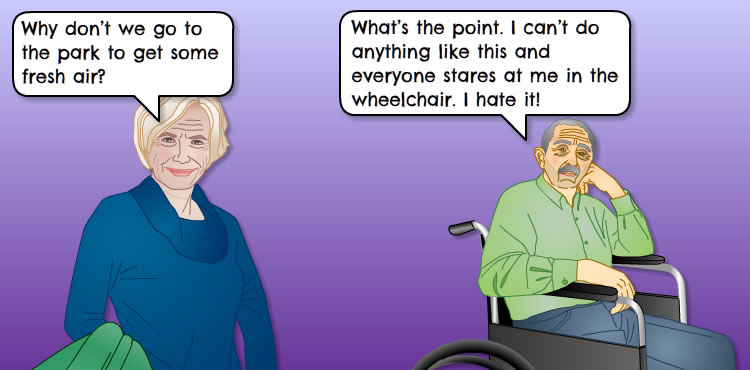

 Alec, 61 years. “If I do more for myself it saves them money, all they want to do is save a pound or two at my expense. Its all about cutbacks, nothing to do with what I want “.
Alec, 61 years. “If I do more for myself it saves them money, all they want to do is save a pound or two at my expense. Its all about cutbacks, nothing to do with what I want “. Agnes, 62 years takes the self management approach: “It’s not just about saving money; I also want to be able to help myself. It’s my responsibility to look after my own health for now, and in the future”.
Agnes, 62 years takes the self management approach: “It’s not just about saving money; I also want to be able to help myself. It’s my responsibility to look after my own health for now, and in the future”.