Since your stroke…….
- Have you ever made up an excuse to avoid meeting a friend?
Feedback – Sometimes it can be difficult to see friends if you are worried about how they will react to you since your stroke.
- Do you avoid answering the phone?
Feedback: You may not like speaking to people on the phone. It is often harder to follow what they are saying and judge their reactions when you can’t see them face to face
- Do you avoid eating in company?
Feedback: If you have problems with eating or swallowing it can be embarrassing if you need to eat more slowly or if you think you make a bit of a mess.
- Have you deliberately avoided someone you know so that you don’t have to speak to them?
Feedback: Speaking with people or even just making ‘small-talk’ takes effort and concentration. You may also want to avoid having to explain what has happened to you
- Have you stopped going to a regular club or social gathering?
Feedback: You may find it easier to speak with people on their own, rather than in a big group.
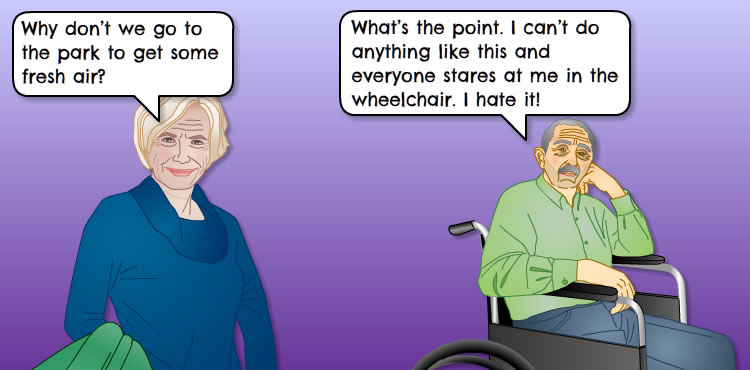
- Are you happy that friends or family do things for you that you could easily do yourself?
Feedback: Allowing family and friends to do things for you means that you can avoid meeting and speaking with other people, perhaps because you don’t like to be seen using a walking stick or you feel flustered in a crowd.
- Do you find yourself working differently for example sending someone else in place of you for meetings?
Feedback: Often a stroke causes tiredness and affects memory and concentration. You may feel out of your depth with the job you did before your stroke.
- Do you have an excuse at the ready to get out of meetings or leave social functions early?
Feedback: You may feel the need to give yourself a way of escaping from situations where you feel anxious or uncomfortable
- Do you use ‘dutch courage’ to help you cope?
Feedback: Sometimes people will use alcohol to try and help calm them if they are anxious or worried (?link to alcohol following a stroke)
- Do you act differently in company?
Feedback: Trying to act differently to how you feel or “putting a face on things” can be very tiring. It can also become increasingly difficult to keep up the façade.
Click here for some feedback
(4- 10 yes – feedback)
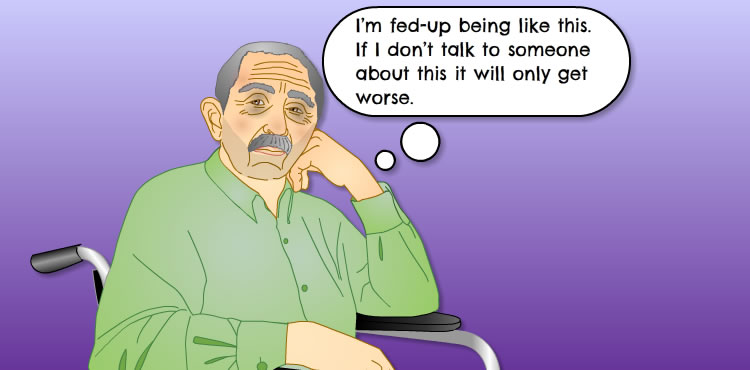
Your answers show that you do sometimes put things off as a means of dealing with difficulties you are experiencing since your stroke. This is common and allows you to cope with the day to day issues that you are finding challenging.
It is good that you have recognised this. You can now use some of these examples in the next section. This may help you in tackling some of these difficulties at a time when you feel ready.
(0 – 3 yes – Feedback)
Your answers show that you occasionally put things off as a means of dealing with difficulties you are experiencing since your stroke. This is common and allows you to cope with the day to day issues that you are finding challenging.
It is good that you have recognised this. You can now use some of these examples in the next section. This may help you in tackling some of these difficulties at a time when you feel ready.
















 “I was told there was nothing more they could do for me, I think they thought I couldn’t get any better, they just abandoned me and left me to do it all on my own ”
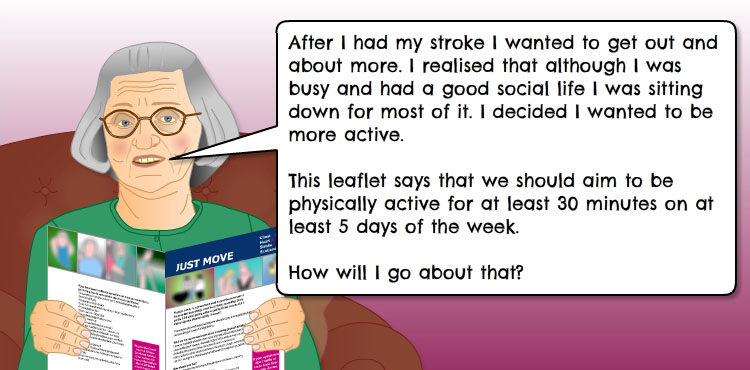
“I was told there was nothing more they could do for me, I think they thought I couldn’t get any better, they just abandoned me and left me to do it all on my own ” Arek, 42 years, takes a self management approach. He had a stroke last year and lost his ability to speak. “The speech therapist took me as far as she could then explained the importance of me carrying on with the support of a communication support service and my family. I have been delighted with the progress I have made – my hard work has paid off.”
Arek, 42 years, takes a self management approach. He had a stroke last year and lost his ability to speak. “The speech therapist took me as far as she could then explained the importance of me carrying on with the support of a communication support service and my family. I have been delighted with the progress I have made – my hard work has paid off.”